A personalized treatment plan
There is no such thing as “one treatment fits all” when it comes to treating myeloma. What works for one person may not work for another, which is why each case must be assessed individually.
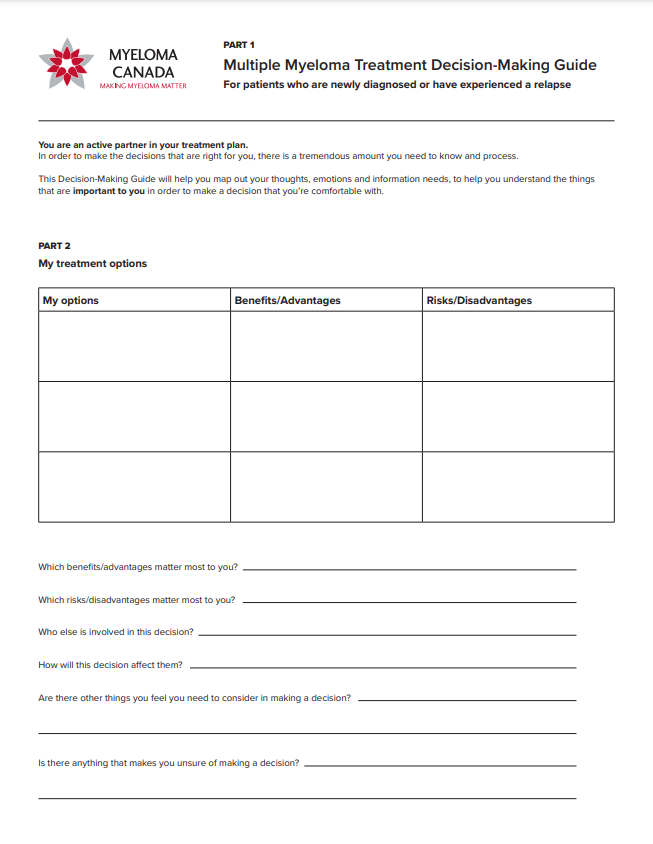
The Treatment Decision-Making Guide can help you map out your thoughts and emotions and identify what’s important to you as you evalute your treatment options.
Access the interactive online formPause, rewind, rewatch
The treatment landscape can be overwhelming.
For a straightforward explanation that you can pause, rewind, and rewatch as often as necessary, watch our Multiple Myeloma Treatment Options video.
Standard types of treatment for myeloma in Canada
Treatment may include a combination of:
- Sometimes the best treatment is no treatment at all
- Monitoring the condition may be the best option for people with:
- MGUS (a precursor of myeloma)
- asymptomaticWhere a person does not experience any symptoms of their condition. or smouldering myeloma (i.e., disease that’s stable or not yet active)
- High-energy radiation may be used to damage the myeloma cells and prevent them from growing;
- Typically used on specific parts of the body, usually in combination with chemotherapy.
- A number of drugs are used, often in combination, to reduce the number of plasmaThe liquid part of the blood in which red blood cells, white blood cells, and platelets are suspended. cells in the bone marrowSpongy tissue that is found inside your bones. It is soft, fatty and full of blood vessels. Your bone marrow is where most of the blood cells in your body are made. and the proteins they produce.
- Chemotherapy does not cure myeloma, but it can put the disease in remission.
- Chemotherapy is tailored individually to each person and is usually administered in cycles of alternating treatment and rest periods.
- Steroids may be used to help prevent inflammation, either alone or in combination with other drugs such as chemotherapy drugs.
- If eligible, there are 2 main types of stem cell transplant approaches people with myeloma may undergo: 1) autologous or 2) allogeneicSee "Transplantation." stem cell transplants.
- Autologous stem cell transplant (ASCT) – The person’s own stem cellsThe immature cells from which all blood cells develop. Normal stem cells give rise to normal blood components, including red cells, white cells and platelets. Stem cells are normally located in the bone marrow and can be harvested for transplant. are collected, frozen, and stored until it’s time for them to be reinfused into their body. ASCT is the standard of care and most commonly used therapeutic approach for newly diagnosed transplant-eligible people with myeloma.
- To prepare for an ASCT, the number of myeloma cells needs to be reduced. This is often done with an “induction regimen” most often using a bortezomib-based combination such as CyBorD (cyclophosphamide, bortezomib, [eg, Velcade] and dexamethasone).
- The stem cells are collected, frozen, and stored until it’s time for them to be reinfused.
- Before the transplantation, patients undergo a “conditioningTreatments used to prepare a patient for stem cell transplant that may include chemotherapy, immunotherapy and radiation to the entire body. Conditioning regimens help make room in the patient's bone marrow for new stem cells to grow and help kill cancer cells that are in the body. regimen” consisting of high-dose chemotherapy with melphalan (eg, Alkeran) to destroy cancerA term for diseases in which malignant cells divide without control. Cancer cells can invade nearby tissues and spread through the bloodstream and lymphatic system to other parts of the body. cells and blood-producing cells in the bone marrow. Then, the transplanted stem cells can begin to produce new blood cellsMinute structures produced in the bone marrow; they include red blood cells, white blood cells, and platelets..
- Allogeneic stem cell transplant – This approach is generally only undertaken under the supervision of a clinical trialResearch studies done with patients to evaluate new treatments or new ways of combining and administering existing treatments. By testing new drugs or combinations of drugs, each study is designed to find better ways to treat the disease, as well as improve quality of life and answer scientific and clinical questions. The overall goal of conducting clinical trials is to improve patient care and outcomes. setting. In allogeneic stem cell transplants, the stem cells come from a matching donor such as a relative (usually a sibling), or a matched unrelated donor (MUD).
There are also other potential types of stem cell transplantation approaches that may be used to treat myeloma such as tandem (double) transplant.
- Maintenance therapy is a prolonged and often low-dose form of treatment that can be given to people with myeloma after an autologous stem cell transplant.
- The goal of maintenance therapy is to prevent disease progressionWhen a disease or physical ailment's course worsens, grows or spreads. for as long as possible while maintaining a good quality of life.
- Consolidation therapy involves a shorter course of treatment with the goal of deepening response to initial therapy.
- Clinical trials are research studies where selected participants may be given new drug therapies that are in various stages of development and not yet available to the general myeloma population. Because people are involved, all clinical trials in Canada must be reviewed by Health Canada and shown to be safe.
- Clinical trials must also be approved by the ethics committees of all participating hospitals. These review processes are in place to protect the safety of participants.
- Only studies that pass these rigorous approval processes are allowed to recruit patients.
People living with myeloma may also be prescribed other supportive treatments to:
- help prevent or manage potential side effectsProblems that occur due to drugs used for disease treatment. Common side effects of cancer treatment are fatigue, nausea, vomiting, decreased blood cell counts, hair loss, and mouth sores. of treatment combinations;
- treat the symptoms and complications of myeloma, such as pain, bone disease, anemia, etc.

Stem cell transplant eligible vs. Stem cell transplant ineligible
Being stem cell transplant ineligible does not mean that you don’t have treatment options. Thanks to advances in research, there are more new and promising treatments than ever. Also, depending on the specifics of your disease and experience, you may be eligible to participate in a clinical trial.
Learn more in our High-Dose Therapy and Autologous Stem Cell Transplantation InfoGuide.
Order a printed copyHigh-dose chemotherapy with stem cell transplantation
It’s normal to feel anxious about undergoing a stem cell transplant. Learn more about the experience from others in your situation by watching their personal journey video.
Learn more about stem cell transplantation and why it might be recommended for you. Watch our educational Multiple Myeloma Stem Cell Transplant video.

Treatment and possible side effects
There are various drug therapies for myeloma. How your body responds to these will be particular to your personal circumstances. However, there are some treatment side effects and complications due to the disease that you should be aware of, including:

Experiencing a relapseThe reappearance of signs and symptoms of a disease after a period of improvement. can be difficult. Learn more from others who have gone through it.
You and your medical team
A cancer diagnosis can leave you feeling terribly alone. Chances are, the news came as a shock. This is even more true when you’re diagnosed with a cancer you may have never even heard of before, and now you feel like you’re starting the fight of your life.
The truth is, you are not alone. You’ve got an entire team of dedicated professionals in your corner, ready and willing to help in any way they can.
In this section, we’ll introduce you to the professionals who may be part of your healthcare team, the roles they each play, and how you can best communicate with them so you can be a more informed and active participant in your own care.
Your medical team may include
Your family doctor was probably the first person you saw when you became ill or started to experience myeloma symptoms. They may have narrowed down possibilities of a diagnosis and may have referred you to a specialist for more specific tests. Most family physicians treat only a few, if any, myeloma patients in their practices.
A medical oncologist is a physician who specializes in the diagnosis and treatment of cancer. As such, they may be the key member of your healthcare team and will determine your exact diagnosis. In consultation with other specialists, your oncologist will most probably design your treatment plan.
Because myeloma is a cancer of the blood, you may be referred to a hematologist, a specialist who studies, diagnoses, and treats blood diseases and disorders. They too may be a key member of your healthcare team. Some hematologists specialize in blood cancers, while others may specialize in other blood problems such as clotting disorders.
If you require radiation therapy, you’ll be referred to a radiation oncologist. As the name implies, a radiation oncologist is a physician who specializes in treating cancer with radiation therapy.
Questions to ask your oncologist, hematologist, and/or radiation oncologist
- Who should I contact if I have problems, especially after hours or on weekends? Be sure to ask for names and telephone numbers.
- What are the results of my tests? What do those results mean?
- What are my treatment options? Which ones do you recommend? Why do you feel this is the best approach?
- Are there any clinical trials available either at this centre or other centres that I might consider?
- What should I expect when undergoing treatment?
- How will we know if the treatment is working?
- Are there any warnings or side effects I should watch out for? If they occur, to whom should I report them? Which ones do I need to report immediately?
- Are there foods, vitamins, supplements, or herbal therapies that I should avoid?
- Are there any special foods, vitamins, supplements, or herbal therapies that could help?
- How often will I require testing and/or follow-up care?
A surgical oncologist is a surgeon who specializes in cancer surgeries. For example, if you need to have a tumour removed, you may be referred to a surgical oncologist.
If you require surgery on your bones, muscles, or joints, you may be referred to an orthopedic surgeon.
Questions to ask your surgical oncologist or orthopedic surgeon
- Can you explain my surgical procedure in detail?
- What should I expect before, during, and after surgery?
- What will my recovery be like?
- When should I come back for a follow-up visit?
There are several roles nurses may play in your healthcare team.
- Oncology nurse – a specially trained nurse who works closely with your medical oncologist, hematologist, or radiation oncologist to coordinate your care, oversee your therapy, and keep your healthcare team informed of any problems you may encounter.
- Nurse practitioner – a nurse who has completed additional training in the diagnosis and treatment of medical conditions.
- Other nurses may also specialize as cancer educators.
Questions to ask your cancer nurse, nurse practitioner, or educator
- What is your role in my cancer care? Are you the person I should contact if I have a problem or question?
- Can you help me find reliable and accurate information on myeloma?
- What advice can you give me at this stage of my cancer treatment?
- What sort of activities can you suggest so I can stay as active as possible? Which activities should I avoid?
Your myeloma treatment may involve many medications. Some may be oral, while others may need to be delivered intravenously. Pharmacists, whether they work in the hospital or in the community, are an invaluable source of information for you and your caregivers. They can help you understand the medications you’ve been prescribed, how they work, how to take them, what you can expect while taking them, and what to do if side effects occur.
Questions to ask your pharmacist
- Why was this medication prescribed? What is its purpose? What side effects are likely to occur, and which ones should I report immediately if they do occur?
- Are there other medications, vitamins, supplements, and/or herbal remedies that I should avoid while taking this drug?
- Can you help me set up a system, such as daily pill boxes or blister packs, to help ensure I take all my medications as prescribed?
Your dentist is an important but often overlooked member of your healthcare team. Good oral health is more important than ever when you’re being treated for myeloma since infections in your teeth drain into the lymph glands in your neck. This means that if your teeth and gums are not kept clean, bacteria can multiply and settle in your gums and cause serious infections, which could otherwise be easily prevented.
The best time to identify and treat dental problems is before you start chemotherapy, undergo a stem cell transplant, or start taking bisphosphonates. You may have to take antibioticsDrugs used to treat infection. as a precaution before undergoing dental treatment, especially if you have a central line or catheterA tube that is placed in a blood vessel to provide a pathway for drugs or nutrients. A Central Venous Catheter is a special tubing that is surgically inserted into a large vein near the heart and exits from the chest or abdomen. The catheter allows medications, fluids, or blood products to be given and blood samples to be taken. in place.
Dentists who work in cancer centres are familiar with the special requirements of myeloma patients but dentists who work in the community may not be. Make sure your dentist is aware of any drug you’re taking (including intravenous therapies), where you are in your therapy, and of any future treatment plans you may already know of. It’s also a good idea to encourage your dentist to talk to your cancer specialist.
Questions to ask your dentist
- Are there any infections or dental problems that should be taken care of before I begin my myeloma treatment?
- Are you familiar with the requirements for treating someone with myeloma and/or with a central line in place?
- What can I do to reduce the likelihood of extractions or other traumatic dental work while I’m undergoing treatment?
Cancer and its treatment can often make eating difficult. Sometimes eating enough or eating the right kinds of food to keep up your strength can be a challenge.
Or you may experience the opposite and find it hard to avoid overeating because certain medications may increase your appetite. A registered dietician or nutritionist can help you maintain the healthiest diet possible as you go through the different stages of your myeloma journey. If you’re experiencing nausea, vomiting, loss of appetite, or a dry or sore mouth, they can suggest foods or drinks that may help.
Questions to ask your dietician or nutritionist
- I’m finding it difficult to eat. Is there anything you can recommend to help me? Are there any foods or drinks I should avoid?
- I’m about to start a new therapy. What is known about this treatment’s effect on appetite, digestion, etc.? Is there anything you can recommend to reduce its effects?
- My appetite has increased since I’ve started taking steroids, and I’m finding it hard to control my eating. What should I do?
A psychiatrist is a medical doctor who specializes in the diagnosis and management of mental illness. A psychologist is a professional who has undergone advanced training in counselling and human psychology, but is not a physician.
Both psychiatrists and psychologists can be very helpful in dealing with the psychological, emotional, and behavioural issues you may face. In addition to “talk therapy,” psychiatrists are licensed to prescribe medication, if required.
Questions to ask your psychiatrist or psychologist
- Can you help me better deal with the emotional effects of my diagnosis?
- My family members and loved ones are very upset about my illness. How can I help them?
Like a psychologist, a social worker or counsellor can help you deal with the many emotional changes that can result from being diagnosed and living with myeloma. A social worker may also be able to help you deal with some of the practical issues that can arise, such as finding out more about your healthcare coverage.
Questions to ask your social worker or counsellor
- Can you help me and my family learn ways of coping with the changes brought on by myeloma?
- Can you help me figure out healthcare or other benefits (for example, short- or long-term disability leaves) for which I may be eligible?
A physiotherapist is a healthcare professional trained to help people restore, maintain, and maximize their strength, function, movement, and overall well-being. For people living with cancer, and myeloma specifically, consulting with a physiotherapist may help manage pain and improve mobility. It’s important to make sure your physiotherapist has experience in treating people with myeloma.
Other support
Some people find it helpful and comforting to talk with a member of the clergy or a spiritual advisor.
Questions to ask your clergy member or spiritual advisor
- Can you help me better deal with the emotional effects of my diagnosis?
- My family members and loved ones are very upset about my illness. How can I help them?
Support groups can be invaluable as you learn to cope and live with a myeloma diagnosis. Not only do they provide important information about myeloma and its treatment, but they’re a safe space to meet and share with others who understand first-hand the journey you’re on.
Myeloma Canada has a vast network of community-based support groups across Canada, virtual (Facebook) support groups, and peer support programs.
For more information on how to pepare for appointments, visit

To help you manage, track, and organize your journey with myeloma, download Myeloma Canada’s award-winning Myeloma Monitor.